In the realm of healthcare, artificial intelligence (AI) stands as a beacon of transformative potential, heralding a future where diagnostics are more precise, treatments more personalized, and preventive measures more effective. As we stand on the cusp of this new era, AI's integration into healthcare promises not only to enhance patient outcomes but to reshape the very fabric of medical practices. From leveraging deep learning for early disease detection to employing sophisticated algorithms for drug discovery, AI's applications are broadening horizons, promising a future where healthcare is more accessible, efficient, and tailored to individual needs.
Present Applications
Disease Diagnosis
AI algorithms, particularly those based on deep learning, are increasingly accurate in diagnosing diseases from imaging data. For example, AI can interpret X-rays, MRIs, and CT scans to detect anomalies like tumors, fractures, or diseases such as pneumonia.
In the field of hematology, AI is revolutionizing diagnostics through advanced image processing and machine learning (ML) techniques. Techniques like support vector machines, random forests, and artificial neural networks (ANN) classify various cell types. This automation extends to peripheral blood and bone marrow smears, where AI helps in pre-screening and interpreting complex images. For more detailed insights, you can explore the comprehensive study on this topic in the article "How artificial intelligence might disrupt diagnostics in hematology in the near future" on Nature's website.
Personalized Medicine
AI analyzes data from various sources, including genetic information, to tailor treatment plans to individual patients, enhancing the effectiveness and reducing side effects.
Personalized medicine, also known as precision medicine, tailors medical care to the individual, leveraging genetic and genomic information to guide decisions on disease prevention, diagnosis, and treatment. This approach has roots in advancements like the Human Genome Project. Examples include using family history and genetic testing for conditions like Lynch syndrome, hereditary breast, ovarian, and prostate cancers. Additionally, targeted therapies, such as imatinib for chronic myelogenous leukemia, exemplify personalized medicine's application in treating cancer.
Robot-Assisted Surgery
Robot-assisted surgery has significantly advanced the field of minimally invasive procedures, allowing surgeons to perform complex operations with higher precision, flexibility, and control. This technology, widely exemplified by systems like the da Vinci Surgical System, includes a camera arm and several mechanical arms with surgical instruments attached, which the surgeon controls from a console providing a 3D, high-definition, magnified view of the surgical site.
The scope of robot-assisted surgeries spans across various medical disciplines, including urology, gynecology, general surgery, cardiothoracic surgery, and colorectal surgery. Procedures such as heart surgeries (e.g., atrial septal defect repair, mitral valve repair), gastrointestinal surgeries (e.g., colectomy, gastrectomy), and urologic surgeries (e.g., cystectomy, radical prostatectomy) are just a few examples of the operations being performed with robotic assistance.
The advantages of robotic surgery over traditional methods are substantial. They include smaller incisions, resulting in less pain and quicker recovery times for patients, as well as reduced blood loss and lower risk of infection. However, it's important to note that robotic surgery may not be suitable for everyone and is typically performed by surgeons who have undergone specialized training in robotic systems.
Virtual Health Assistants
Virtual Health Assistants (VHAs) are playing an increasingly important role in transforming healthcare by providing support that makes healthcare management easier, faster, and more efficient. VHAs are equipped with a variety of capabilities, such as understanding complex health-related inquiries through Natural Language Processing (NLP), handling administrative tasks, and providing personalized health advice. They can offer reminders and alerts for medication, appointments, and exercise routines, and even support mental health through resources for managing anxiety and depression. Furthermore, VHAs can connect with wearable devices to offer more personalized health suggestions and play the role of a virtual nurse, providing medical advice and scheduling appointments.
In addition to aiding in patient care, VHAs can also assist healthcare professionals by providing instant access to comprehensive medical databases and calculators, integrating data from third-party clinical tools, and supporting evidence-based decision-making. They can automate the process of remote patient monitoring and follow-ups, allowing clinicians to serve more patients efficiently.
Predictive Analysis
Predictive analytics in healthcare is increasingly being used to improve patient outcomes, streamline hospital operations, and reduce healthcare costs. Examples include early detection of patient deterioration in ICUs and general wards, where predictive algorithms analyze continuous monitoring data to identify patients who may require urgent intervention, potentially reducing adverse events and cardiac arrests significantly.
In disease management, healthcare institutions utilize predictive analytics to foresee the progression of conditions like diabetes into renal disease or the onset of sepsis, allowing for early interventions that can drastically improve patient outcomes. Predictive analytics also plays a crucial role in managing hospital resources by forecasting patient stays and readmission risks, enabling adjustments in care protocols to avoid unnecessary overstays and optimize resource allocation.
Moreover, predictive analytics extends its benefits beyond clinical settings by identifying maintenance needs of medical equipment like MRI scanners before they arise, ensuring operational efficiency and minimizing disruptions. This approach mirrors practices in industries like aviation, where predictive maintenance has long been standard, and is now being applied in healthcare to anticipate and prevent equipment failures, thereby ensuring uninterrupted patient care.
Near Future Applications
Early Detection of Diseases
Early detection of diseases, especially cancer, is crucial for improving treatment outcomes and survival rates. Advances in technology, particularly artificial intelligence (AI), have significantly enhanced the early detection of various illnesses. For example, AI has been applied to improve the accuracy and efficiency of diagnosing diseases through the analysis of medical imaging, such as mammograms for breast cancer detection, potentially outperforming traditional methods used by radiologists. This approach not only aids in identifying tumors at an early stage but also contributes to the development of personalized healthcare by tailoring treatment plans to individual patients based on their specific disease characteristics.
Moreover, predictive analytics in healthcare is being utilized to forecast disease progression and identify patients at risk of developing comorbidities, such as renal disease in diabetes patients or sepsis in hospitalized individuals. This capability allows healthcare providers to intervene earlier, significantly improving patient outcomes. Predictive models also assist in managing hospital resources more efficiently by forecasting patient stay durations and readmission risks, enabling more effective care protocols and reducing unnecessary healthcare costs.
Enhanced genomic analysis
Enhanced genomic analysis is revolutionizing healthcare by enabling more precise and personalized medical interventions. One significant example is the All of Us Research Program, which utilizes AI and cloud computing to make a vast array of biomedical data, including genomic information, available to researchers. This initiative, in collaboration with Intel and Google Cloud, aims to accelerate research not only for COVID-19 but for a broad spectrum of diseases by making genomic and EHR data more accessible.
Institutions like the University of Utah are collaborating with companies like Renalytix AI to leverage data-driven analytics for identifying genetic biomarkers of diseases. Such partnerships are pivotal in advancing precision medicine, especially for conditions like diabetes and kidney disease, by utilizing genomic data to inform diagnosis and treatment protocols.
Furthermore, initiatives like the Multimodal Biomedical AI and the Project Baseline Health Study are collecting and analyzing multimodal data, including genomic information, to understand diseases better and develop targeted treatments. These projects exemplify the move towards integrating various data types, such as EHR, imaging, and genomic data, to improve diagnostic accuracy and patient care.
The National Human Genome Research Institute (NHGRI) highlights the growing impact of genomic medicine across various medical fields, including oncology and pharmacogenomics. Genomic medicine, a subset of precision medicine, is increasingly being incorporated into clinical practice to guide diagnosis and tailor treatment strategies based on an individual's genetic makeup.
Automated health records
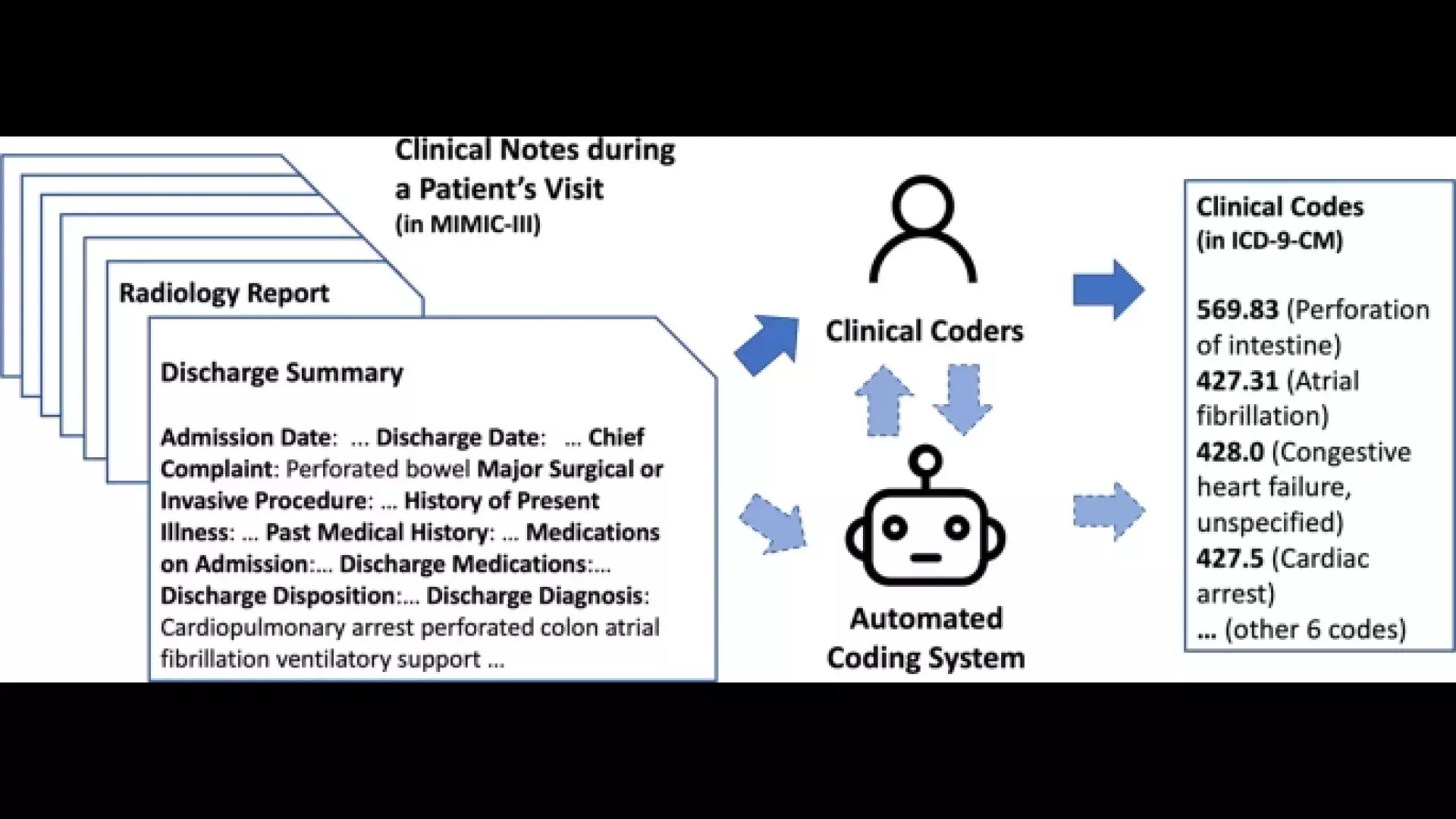
Automated health records are transforming healthcare by streamlining administrative tasks, enhancing data accessibility, and improving patient care. For instance, artificial intelligence and machine learning technologies are being integrated into electronic health records (EHRs) and other healthcare systems to automate tasks like worklist optimization and hanging protocols in radiology, thereby enhancing workflow and productivity for radiologists and administrators. This integration not only benefits patient care but also boosts clinician and staff productivity, contributing to the profitability of healthcare organizations or radiology reading groups that serve them.
The complexity of clinical coding, a crucial part of health records management, presents significant challenges for automation due to the nuanced understanding required of clinical documents and the dynamic nature of classification systems like ICD-10 and ICD-11. Automated clinical coding involves natural language understanding and linking clinical text to complex classification systems, which is a non-trivial task given the variability and structure of clinical documentation.
Moreover, automation in healthcare extends beyond clinical documentation and coding. It encompasses various operational and administrative areas, offering benefits such as easier scheduling, cost reduction, easy data transfer and access, fewer errors, and improved handling of emergencies and adaptations to change. For example, appointment scheduling software automates the booking process, reducing scheduling conflicts and administrative overhead. Automated data transfer systems enhance inter-departmental communication and patient care by making patient data readily available across different healthcare units. Furthermore, automation can lead to cost savings by reducing the need for overtime and minimizing errors, thereby improving the overall efficiency of healthcare facilities.
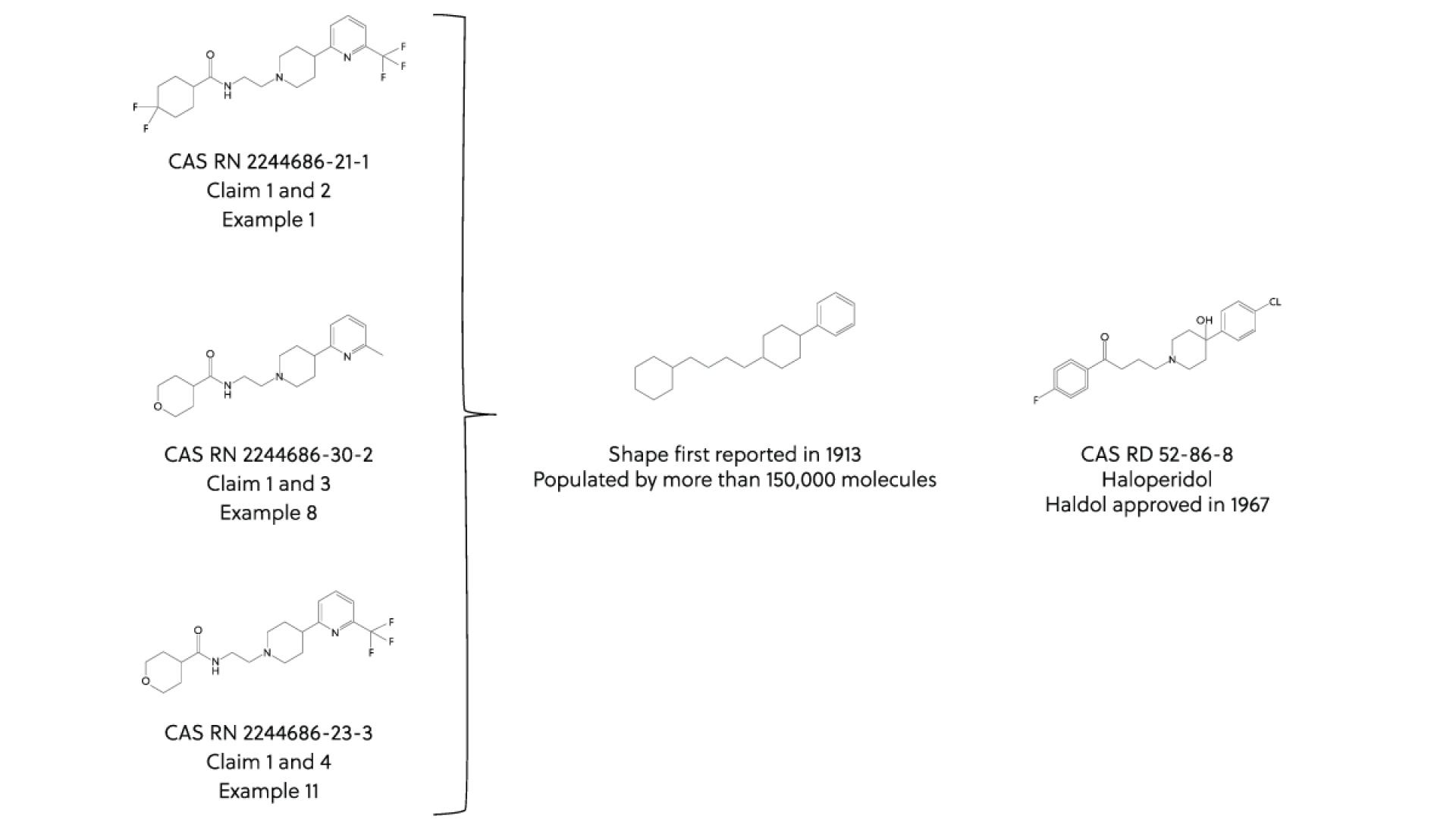
Drug Discovery and Development
AI is increasingly being utilized in the drug discovery and development process, offering a new wave of innovation and efficiency in the pharmaceutical industry. For example, AI can enhance small-molecule drug discovery by providing access to new biology, improving chemistry, increasing success rates, and making the discovery process quicker and cheaper. AI-native companies are leading much of this progress, using data and analytics to improve specific use cases within the drug discovery value chain, such as target discovery, validation, and small-molecule design. Large pharmaceutical companies have gained access to these capabilities through partnerships or software licensing deals, applying them to their own pipelines.
One of the pivotal moments in AI-driven drug discovery was when the first AI-designed drug candidate entered clinical trials in early 2020, as reported by Exscientia. Following this, several companies, including Insilico Medicine, Evotec, and Schrödinger, have announced phase I trials for candidates developed using AI-enabled solutions. This marks a significant milestone, demonstrating the capability of AI to accelerate clinical development and potentially bring novel therapies to market more efficiently.
AI's impact in drug discovery is substantial, enabling the creation of structurally novel molecules that are more likely to lead to promising new therapies. For instance, the AI-designed drug candidates DSP-1181, EXS21546, and DSP-0038, which are in Phase 1 trials, were discovered using Exscientia’s AI platform. These candidates illustrate the potential of AI to innovate in molecule design and target novel biological pathways.
Remote Patient Monitoring (RPM)
Remote Patient Monitoring (RPM) has become an increasingly valuable tool in healthcare, allowing for the monitoring and management of patients' health conditions from the comfort of their homes. This approach has shown particular utility in specialties like cardiology, pulmonology, and endocrinology, among others.
In cardiology, RPM is used for hypertension management by regularly monitoring blood pressure with at-home devices that transmit data directly to healthcare providers. This continuous stream of data enables more precise management of the condition, including medication adjustments. RPM also plays a critical role in managing congestive heart failure (CHF) through daily weight monitoring, which can indicate fluid retention, a common symptom of CHF. By identifying these changes early, healthcare providers can intervene more quickly, potentially reducing hospitalizations.
Pulmonology has also seen significant benefits from RPM, particularly in the management of chronic obstructive pulmonary disease (COPD) and asthma. RPM devices allow for regular monitoring of lung function and symptom management, providing valuable data that can lead to adjustments in treatment plans and improved patient outcomes. During the COVID-19 pandemic, the value of RPM has been further highlighted, enabling the monitoring of patients with respiratory conditions without the risk of exposure to the virus.
Endocrinology benefits from RPM through glucose monitoring for diabetes management. Devices such as blood glucose meters and continuous glucose monitoring systems (CGMs) enable regular tracking of blood sugar levels. This continuous data collection helps in making informed decisions regarding medication adjustments and lifestyle changes to better manage diabetes.
The Mayo Clinic's Remote Patient Monitoring Program exemplifies the comprehensive application of RPM, particularly in response to the COVID-19 pandemic. Patients diagnosed with COVID-19, especially those at risk for complications, receive at-home monitoring kits that include devices like blood pressure cuffs, thermometers, and pulse oximeters. The data collected from these devices is monitored by healthcare professionals, allowing for timely interventions based on changes in the patient's condition. This program underscores the potential of RPM to provide high-quality care remotely, ensuring continuous patient support while minimizing the risk of virus transmission.
Overall, RPM is reshaping healthcare delivery by enabling more proactive and personalized care, reducing the need for in-person visits, and potentially lowering healthcare costs. As technology continues to evolve, the scope and effectiveness of RPM are expected to expand, further integrating this approach into various medical specialties.
Impact on Patients and Diagnostics
- Accuracy and Speed: AI can process and analyze vast datasets far quicker than humans, leading to faster and often more accurate diagnoses.
- Personalization: Treatments and healthcare plans tailored specifically to the individual will become the norm, improving patient outcomes.
- Accessibility: AI applications, such as telemedicine and virtual assistants, can make healthcare more accessible, especially in remote or underserved areas.
- Preventive Healthcare: With predictive analytics, healthcare can shift from a reactive to a proactive model, focusing on preventing diseases before they occur or become serious.
- Patient Empowerment: AI tools can provide patients with more information and control over their health, leading to better engagement in their healthcare processes.
While the integration of AI in healthcare presents substantial benefits, it also comes with challenges, including ethical considerations, data privacy, and the need for robust validation of AI tools. Balancing innovation with these considerations will be key to realizing the full potential of AI in healthcare.
![[©Wencke Walter et al. Nature] The central part of the figure displays current and future diagnostic tests and methods, while the outer part illustrates the various data types and the potential clinical impact of ML-based applications and analyses. DL deep learning, ML machine learning.](/sites/default/files/public/styles/main_1920pxauto/public/2024-02/41388_2021_1861_fig2_html.webp?itok=bm3JSy9E)